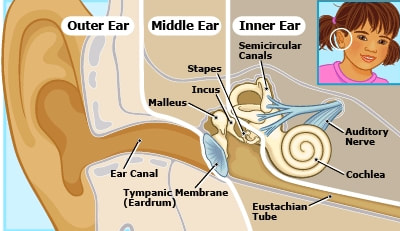
 ©Nemours Health Foundation ©Nemours Health Foundation Ear infections happen when infected fluid builds up in the space behind the ear drum (or tympanic membrane), called the middle ear. Fluid in the middle ear usually drains out the eustachian tubes, which connect the middle ear to the back of the nose. These tubes are soft tubes (like a sock with the toes cut off) rather than a hard tube (like a straw). Eustachian tubes open and let fluid drain from the middle ear when you move your jaw around talking or chewing, when you yawn, or when you hold your nose blow to “pop” your ears. If there is swelling or mucus around the opening of the eustachian tubes, like from allergies or a cold, the fluid can’t drain and will build up in the inner ear. If you have ever had a cold and felt like your ears were “stuffy” or your hearing was muffled, this is probably what was going on. Kids tend to get more fluid behind their ears than adults, because kids’ eustachian tubes are more horizontal. As people get older, their eustachian tubes get more vertical, which makes it easier for the fluid to drain.  Equipment for pneumatic otoscopy Equipment for pneumatic otoscopy As you can see, lots of things make fluid build up behind the ear drum that aren’t necessarily a bacterial infection. This can make ear infections difficult to diagnose. In the past, doctors tended to give antibiotics to every child with ear pain and a red ear drum, but newer research has shown that most ear infections will get better on their own without antibiotics. The current practice guidelines recommend use of pneumatic otoscopy (blowing a little puff of air into the ear) to determine if there is fluid behind the ear drum and to look for a bulging ear drum, with other signs and symptoms, such as pain, fever, and significant redness. A bulging eardrum is one of the physical findings required in most studies to diagnose an ear infection (not just a red eardrum). The other finding is ear discharge without an outer ear infection, indicating that the ear drum has a hole in it. Redness of the ear drum does not indicate an ear infection. The ear drum turns red the same way the skin of the face turns red. If the child is crying or hot (from the environment or from a fever), the ear drum may be red without an infection being present. There are also specific recommendations for treatment based on age and symptom severity. For infants 6-23 months with a mild ear infection in one ear or kids over 23 months with a mild infection in one or both ears, there is an option to observe for 48-72 hours before treating. Studies have found that these kids will often get better without taking any antibiotics, avoiding side effects and risk of developing an antibiotic allergy. Kids with more severe symptoms may be treated immediately. One protocol that has been studied is the safety-net antibiotic prescription (SNAP) or wait-and-see prescription (WASP). In this protocol, kids who do not meet the criteria for immediate antibiotic prescription are given a prescription, but parents are told not to fill it (or told to fill it but not give it) unless symptoms get worse or are not better in 48 hours. Usually only about 1/3 of kids in these studies ever get the prescriptions, and no negative outcomes have been found. Some children (and adults) who have fluid behind the ear drum (whether infected or not) also have significant pain, and it is important to treat that pain, even if not prescribing antibiotics. Sometimes, I see kids in clinic for ear infections with no symptom other than pus draining from their ear, often because they had a bulging ear drum that didn’t cause fever or significant pain before it developed a hole to drain fluid. These ear infections are treated with antibiotics. The hold in the ear drum usually heals on its own within a few months, although your child’s doctor will probably want you to come back in to recheck it. If your child has ear pain and fever, contact their primary care clinic for advice and to see if they need an appointment. A recent study found that almost half of antibiotic prescriptions in urgent care clinics were inappropriate with ear infections being one of the most common reasons for antibiotic prescriptions. Pediatricians spend a lot of time in training learning how to examine kids’ and babies’ ears to diagnose ear infections. Your child’s primary care clinic is the best and most accurate place to get them checked for an ear infection. 2/27/2020 11:30:28 am
Thanks for explaining that a puff of air can be blown into the ear to determine if our ear drum is bulging or has fluid behind it. I've been having pain in my left ear for the last three days and want to go to a walk-in clinic to see if it's an infection. I'm glad I read your article and got a better idea of what to expect from being evaluated. Comments are closed.
|
About the blogA look at some topics in breastfeeding, medicine, and kids health. Archives
December 2019
Categories |
 RSS Feed
RSS Feed